
From a perspective of centuries, humans have never been healthier, wealthier, or more numerous.
In 2015, despite a fast-increasing world population, the proportion of the world living in absolute poverty dropped below 10 percent for the first time in history. In parallel, the last few centuries have seen dramatic improvements in human longevity and declines in infectious illness.
But as the world becomes more well, people–particularly people in the West–seem to be more worried about health and disease, especially about the possibility of global pandemics (that is, widespread outbreaks) of newly emerging infectious diseases. Are these first-world fears? Or is there good reason why everyone should be concerned about coming plagues? And, if so, what should we be doing differently to protect ourselves better from newly emerging diseases?
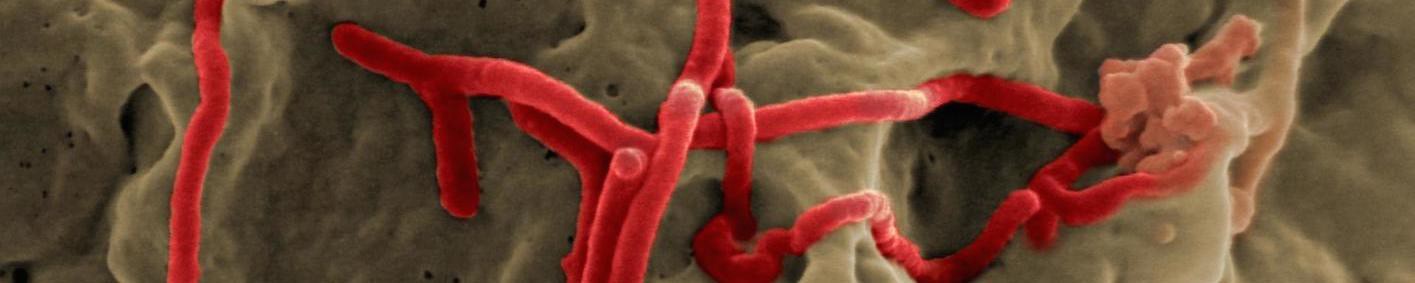
I’m a veterinary epidemiologist working on global “One Health” issues at the International Livestock Research Institute (ILRI), located in East Africa. ILRI’s headquarters lie on the outskirts of the city of Nairobi, Kenya’s capital and home to the highly fatal Nairobi sheep disease. Nairobi was also the origin of several tick fevers and the Kenya tick typhus, which caused skin lesions in people and sometimes death. The country itself is located at the edge of the spectacular Rift Valley, home to Rift Valley fever, the cause of abortions in sheep and hemorrhagic fevers that can kill people. To our east is the beautiful Kenyan coast, breeder of East Coast fever, a cancer-like disease that kills calves as well as adult cattle within three weeks of parasitic infection. Immediately to our west is Uganda, where the Zika virus was first detected in the lush Zika forest. First found in a captive rhesus monkey, caged and placed in the forest to detect yellow fever, the virus is the cause of the globally spreading birth defect known as Zika, or microencephalopathy. Still farther west flows the dark Ebola River, which gave its name to the Ebola virus, the cause of Ebola hemorrhagic fevers that recently killed more than 11,000 people in West Africa.
In all, it’s a good place to be conducting research on neglected and emerging infectious diseases–of animals, people, and pathogen flows between the two.
Researchers in recent decades have worked hard to find ways to prevent or better control such disease pandemics and plagues. One important finding was that most new human diseases–remarkably, at least 75 percent–are zoonotic in origin: that is, the pathogens causing them have jumped from animal to human hosts. A related discovery that most of these new diseases originate in wildlife led to a rush of work to find diseases in wild animals: In deltas and in jungles, in swamps and in forests, the virus-hunters went forth, and wherever they looked, they found. Not surprisingly, they confirmed that people, wildlife, and domestic animals are (metaphorically speaking) swimming together in an invisible sea of viruses, bacteria, and parasites. Many of the microbes they’re finding were previously unknown; most are mobile and potential species hoppers, but probably harmless. A few, however, are catastrophic, even civilization-altering, in their potential to hurt us.
This led researchers like me to ask how we could distinguish among the five nonillions–or 5,000,000,000,000,000,000,000,000,000,000–of microbes in the world (which vastly outnumber any other living organisms and even the estimated star count). We need an approach for identifying those that could cause global pandemics from others that are just harmless hitchhikers.
Here I’m going to focus on domesticated animals, the unacknowledged “Judas sheep” that help microbes leap from their (traditional) wildlife hosts to their (new) human hosts. (The Judas sheep or goat is trained to associate with sheep or cattle, leading them to a specific destination, usually slaughter).
In 2012, the World Bank produced an important study on “big-league zoonoses”: the ones that cost millions to billions of dollars and kill hundreds to thousands of people each year. The study found that of the 11 major pandemics that have afflicted the world since the 1980s–those being Zika, bird flu (highly pathogenic avian influenza, or HPAI), mad cow disease (bovine spongiform encephalopathy, or BSE), Nipah virus infection, plague, West Nile virus, severe acute respiratory syndrome (SARS), Rift Valley fever, Q fever, Middle East respiratory syndrome (MERS), and Ebola–eight have a common feature: They involve domestic animal hosts.
There are good reasons why domestic animals play a major role in transmitting disease: First is that there are simply increasing numbers of them.
Currently, 96 to 98 percent of the planet’s mammalian zoomass is made up of humans and their animals–whether they’re for companionship, sport, work, or part of some 40 billion livestock. Compared to other genetically diverse species, humans and their domestic animals are very genetically similar (especially “out of Africa humans” who appear to have passed through a genetic bottleneck). These virtual clones, human and animal, make an ideal environment for pathogen emergence and spread.
I started by saying that humans today are more numerous and more wealthy than ever before. It’s more people with more money that is driving the increased global consumption of meat, milk, and eggs. The rising demand for livestock products–the so-called “livestock revolution”–has led to the production of ever-greater numbers of animals in “intensive systems” that maximize their production. In these systems, large numbers of animals are raised together in confined spaces. In addition, the animals have been intensively bred and selected to make as much product as quickly (and with as few inputs) as possible.
The result is that today, particularly in industrialized systems, only a very few species and strains of livestock produce nearly all the animal products the world consumes. Among thousands of species of ruminants and omnivores, nearly all of our meat, milk, and eggs comes from just cattle, sheep, goats, swine, and poultry. And even within these we rely on very few breeds. For example, there are nearly 1,000 breeds of cattle but nearly all commercial dairy operation in the world uses just a couple of them (mainly Friesians). The same is true for other livestock–despite the many breeds, a small number dominate while the rest are marginal. The homogenous genetics and confined spaces of industrial production systems together have created a welcome incubator for disease pathogens.

At the same time, some domestic animals are kept in ways that have changed their exposure to wildlife pathogens. For example, keeping pigs in fruit orchards to eat windfalls is a good business model. It’s also a good way to connect (disease-transmitting) fruit-eating bats first with pigs and then with the people who eat them. The same goes for farming wild animals, as happens with civet cats in China. Civet is one of the main ingredients in the exotic wildlife dish dragon-tiger-phoenix soup, for which wealthy Chinese in Guangdong province will pay large sums to eat. But catching wild animals and putting them in close confinement in cages is ecologically unsound, since they are likely to have picked up pathogens in the wild, and the stress of capture and captivity predisposes to disease emergence.
On the other hand, in poor countries where people raise just a few farm animals to improve their livelihoods–and a mix of different animal species are often kept in close proximity to people and households–since veterinary care can be scarce livestock are often sick, malnourished, or immune-suppressed. This also serves as a bridge for pathogen transmission, as well as a crucible for the evolution of newly pathogenic organisms.
By giving greater focus to plagues that pass through livestock, we might better identify the “vital few” from the “trivial many” diseases that are emerging. That in itself would enable rapid responses to disease outbreaks that can stop pandemics, cutting their potential global costs alone by 90 percent.
We’ve already seen that domestic animals can serve as disease bridges–transmitting emerging pathogens from their wildlife hosts, particularly in human-disturbed ecosystems, to human hosts. Like the canary kept in a 19th-century coal mine (the first to die in a poisonous gas event), identifying and investigating ill farm animals should be able help stop disease spread if we let them serve as disease sentinels.
Yet in too many cases, particularly in impoverished nations with fewer resources, we first find out that a zoonotic disease has erupted not when animals begin to die, but when people do. This was the case, for example, with Rift Valley fever in Kenya and bird flu in Sudan. These diseases, which must have felled animal populations long before they started affecting people, were never reported until the first human deaths occurred, by which time the disease was too advanced to be ignored–and too advanced to be easily controlled.
The reason for this is simple. Reporting disease at farm, district, or country levels in the developing world often brings nothing but problems. In response, officials are likely to tell farmers they can’t move or sell their animals, and/or to slaughter their animals, while offering little or no compensation. And among the many poor countries relying on the livestock trade, the last thing they want is news of a new disease in their territory. Changing the incentive structures for reporting livestock diseases, so that people and countries are rewarded instead of punished, would go a long ways toward improving rapid responses to initial disease outbreaks.

Even where disease surveillance is working well, our track record on managing emerging zoonoses is mixed. The rapid containment of sudden acute respiratory syndrome (SARS) in 2003 is certainly one of the biggest success stories in public health in recent years. Within six months of the World Health Organization’s worldwide alert that a severe acute respiratory syndrome of unknown cause was rapidly spreading from Southeast Asia, this entirely new disease was identified as a coronavirus, its transmission and risk factors elucidated, treatments for it developed, and its spread stopped.
The more recent case of Ebola, however, shows that control is not always so straightforward. The Ebola outbreak at the intersection of Liberia, Sierra Leone, and Guinea affected some of the world’s poorest and least developed countries. It took over three months just to confirm that Ebola was the cause of the region’s many severe illnesses and untimely deaths, by which time an immediate response to end the plague was out of the question. West African conflicts, population growth, poverty, and poor health infrastructure–along with delayed global attention–were the toxic mix that encouraged the unprecedented expanse, duration, and size of this Ebola tragedy.
The World Bank estimates that an annual investment of US$3.4 billion in animal health systems would avert economic losses due to delayed or inadequate responses to zoonotic diseases that cost us US$6.7 billion per year. And that does not include the incalculable non-economic losses of human lives and potential. What does this actually mean? Well, for one thing, it suggests that the provision of proactive animal health services would be one of the world’s best investments in the battle against human disease plagues.
A recent economics paper estimates that the cost of future pandemics could be in the same order as that of future climate change. Yet funding for managing pandemic diseases receives only a fraction of that when compared to the investment put toward managing a warming globe. This is deeply worrying. While we humans have historically adapted ourselves successfully to climate change by moving or altering our livelihoods, our responses to plagues to date has largely been to die or flee, with the latter only spreading the plague still farther.
Most people understand that we’re not going to slow climate change, already upon us, without significantly reducing our human-generated emissions of greenhouse gases. I’m arguing here that we’re not going to prevent future catastrophic emerging zoonotic diseases by treating their symptoms. We’re going to have to tackle the root causes of their emergence and confront the fact that human activities are imposing extreme stresses on natural ecosystems. We’ll need to enlarge the focus of our attention on emerging diseases from surveillance, epidemiology, and response (the symptoms) to encompass the fundamental drivers of plague (demography, agriculture, and land-use change).
In summary, the “wellness craze” raging today in the world’s more privileged communities is most likely to be upended not by those things these communities worry most about–pollution or climate change or carcinogens or chronic disease–but rather by a microbe. Preventing future global plagues, whether merely catastrophic in nature or civilization-altering in scope, depends largely on our adhering to three imperatives, all of them focused on livestock. We must attend to the (frequent) sources of zoonoses in domestic animals, reward rather than punish timely animal disease reporting, and address the underlying causes of plagues emerging from livestock.

How We Get To Next was a magazine that explored the future of science, technology, and culture from 2014 to 2019. This article is part of our Vital Signs section, on the future of human health. Click the logo to read more.
